Ensuring Proper Evaluation and Management (E/M) Coding at different Levels of your Healthcare Organization
Electronic health records (EHRs) are widely used by providers and physician practices. These EHRs are programmed to automatically select E/M codes based on documentation. Although the EHRs are of great value, providers should review guidelines with physicians and coders of the organization to ensure error-free coding and achieve proper reimbursement and quality scores.
Guidelines
- Evaluation and Management guidelines 1995
- Evaluation and Management guidelines 1997
- Evaluation and Management Services Information
- Problem list guidelines in EHR
E/M Coding Process
E/M coding designates the level of care for each patient-physician encounter and translates them into five-digit current procedural terminology (CPT) codes to facilitate billing. Each of the levels of care has a designated CPT code. CPT codes are submitted to insurers for payment. There are individual CPT codes for each billable procedure.
E/M at the Physician Levels
Establishing Medical Necessity for a Medical Decision Making (MDM)
Clear and concise documentation of medical records is critical to medical decision making. It forms the basis for continuity of patient care to the correct levels of service. It helps in the correct evaluation and management (E/M) codes for physician-patient encounters.
The documentation for E/M services is based on 3 "key" components. History, Physical exam, and medical decision making.
To document additional levels of complexity, the following key levels are used:
|
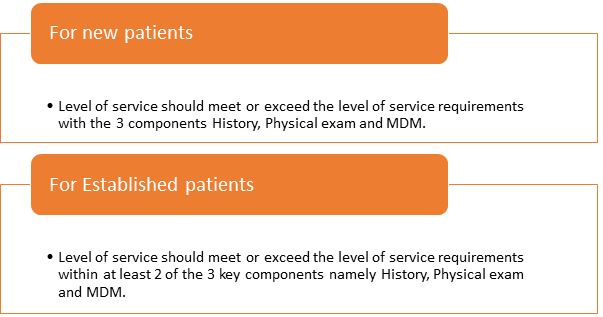
Documentation of the above requirements determines the medical necessity. It's not the volume of documents that justify a higher level of service. Rather, it's the medical necessity that rationalizes the level of service provided. For example, if a test is ordered, the medical document should explain why the decision of ordering the test was taken to establish the medical necessity.
E/M at the Coders' level: Taking time to examine details
Coders should take time to examine the medical documents to see what tests are performed, the reasons for the test, and verify if the provider has documented the rationale for the test. Services should neither be downcoded or upcoded. A coder should not just go by the automated assignment of codes, but should pay attention to the details.
With value based reimbursement on the rise, it's the right time now to ensure proper E/M coding.
To take a deep dive into the Compliance requirements for E/M, attend this in-person seminar 'Coding Evaluation and Management (E/M) From a Physician's Perspective' The speaker C.J. Wolf, MD, M.Ed. has been involved in healthcare for over 20 years beginning with his years in medical school. Apart from teaching about E/M categories, and key components of E/M services, he will provide details about proposed 2019 changes to E/M guidelines.






