Maximizing Reimbursement With Accurate Clinical Documentation and HCC Coding
The basis for Reimbursements
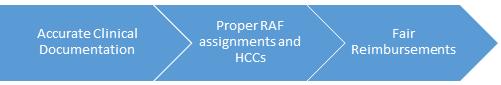
The CMS uses The Hierarchical Condition Category (HCC) risk adjustment model to estimate the predicted cost for Medicare beneficiaries. The HCC assigns each patient a Risk Adjustment Factor (RAF). RAF is a relative measure of the probable costs of care for the individual patient. The reimbursement a Healthcare organization receives for patients enrolled in a Medicare Advantage plan depends on the HCC results. CMS requires the provider organization to identify qualifying conditions each year.

The importance of Accurate Clinical Documentation and HCC Coding
- Accurate Clinical Documentation is essential to the assignment of a correct RAF Score
- Accurate Clinical Documentation improves HCC coding
- Error-free HCC coding positively impacts reimbursements
Common reasons for Inaccuracies
- Failure to include detailed diagnosis while entering billing codes Providers usually capture detailed in-visit notes and diagnosis. But, when entering billing codes, they fail to include these diagnoses in the final claim for that visit. As a result, they are neither counted towards that patient's annual HCC total. Whether in inpatient, outpatient or office settings, a comprehensive process that captures complete HCC and RAF scores for a broad patient population should be established.
- Failure to train staff Concepts of HCCs and their usage in healthcare payments should be understood by physicians, coders and office staff. Providing role based training can offset inaccuracies.
- Failure to involve staff Reviewers and care managers can be tasked with monitoring and analyzing ongoing claims for every patient encounter, and identify missing HCC diagnoses for each patient. Administrative office staff can be involved in patient level population management to improve care coordination and HCC status tracking. When an organization fails to involve and engage staff, inaccuracies can occur.
Best Practices for HCC capture process for your organization's patient population
- Ensure that your clinical documentation and coding reflect HCC risk scores for the patient population based on relevant diagnoses
- Identify if there are gaps in capturing diagnosis and fix them
- Ensure that physicians routinely capture complete HCC-relevant diagnosis information on their patients
- Ensure that physicians have clear information on key diagnoses to address and document for each patient
- Ensure that the documented diagnoses are submitted for billing
- Ensure sufficient coding processes for capturing all relevant HCC diagnosis.
- Train your staff on HCCs
- Establish workgroups responsible for improving responsible documentation and HCC coding
- Monitor and analyze the process for further improvement
To succeed in today's value-based reimbursement (VBR) environment, it is important that the Hospital and Clinic Coding Staff, Managers, Directors, Auditors, CDI Staff, Clinicians, Coding Compliance and Privacy Staff understand HCCs. To this end, you may wish to attend this detailed webinar ‘Compliant HCC Coding and Auditing - What you need to know?. The instructor Victoria is an RHIA (Registered Health Information Administrator), a Clinical Documentation Improvement Practitioner (CDIP), Certified Coding Specialist (CCS), a Certified Coding Specialist Physician-Based (CCS-P) and an AHIMA-Approved ICD-10-CM/PCS Trainer with over 24 years experience in the healthcare field.
You may also wish to browse through our library of healthcare compliance webinars.






