What Case Managers Need to know to Effectively Care for Patients and their Support Systems
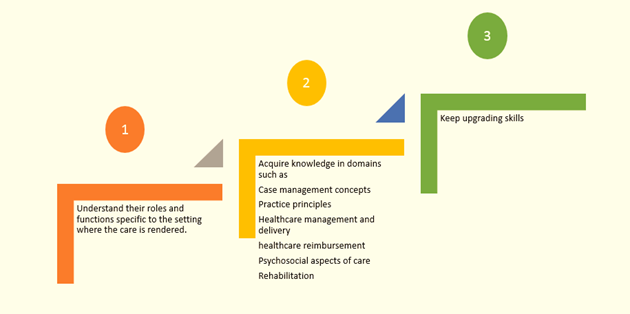
Whether you are an established or an aspiring case manager, learning what you need to succeed in your career will equip you for greater performance. The healthcare landscape is rapidly changing and so is the role of case management in that landscape. In such a rapidly changing healthcare environment, case managers must go through the 3 steps outlined below:
This article discusses the roles and functions of case managers in different settings and guides you to useful case management resources for greater performance.
Understanding the roles and functions of a case manager
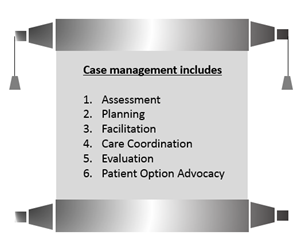
The Case Management Society of America defines case management as 'a collaborative process of assessment, planning, facilitation, care coordination, evaluation and advocacy for options and services to meet an individual's and family's comprehensive health needs through communication and available resources to promote patient safety, quality of care, and cost effective outcomes.'
Case managers practice case management in various settings:
- Physician's office, clinic or other pre-acute setting
- Hospitals
- Acute Inpatient Rehabilitation
- Payer-based setting (Insurance Company)
- Palliative care, home care and hospice case managers play a dual role - that of a caregiver and case manager
- Workers Compensation Case Management focuses on vocational activities, working with the employer to get the employee back to work.
Although the basic role of a case manager is the same, the functions are specific to the settings in which the services are rendered.
The functions of a case manager in different settings.
Case manager at physician's office, clinic other pre-acute setting
The function is primarily focused on preventive healthcare such as
- Wellness programs
- Screenings
- Health risk assessments
- Risk-reduction strategies
- Telephonic triage
- Disease management
- Facilitate access to services
- Referrals to community based resources
- Coordination of medical and social services
- Ensure patient knowledge and compliance with treatment
Case manager at a Hospital
Case management departments are highly crucial to the hospital and to the patients.
Hospitals that integrate case management across the continuum have found that the case management can serve as the lynch pin that connects departments and disciplines across the continuum while retaining the patient as the center figure in the process.
When a patient enters a hospital, they are faced with many tests, staff interactions and paperwork. Especially, during a time when they are sick, thinking clearly is a challenge. Some patients make not have the necessary education to completely comprehend their situation. Such circumstances may be overwhelming. That's where the case manager comes in.
Case managers are advocates for the patient. They liaison between the patient and the health personnel who will treat them. They explain the available options to the patient in simple terms, ease the process through frequent interactions and also involve with the patent's discharge and recovery to complete the process in a safe and timely manner. He determines the patient's continuing medical needs and puts in place a plan in place to meet those needs through discharge planning. Case managers are experts in organizing complex care needs across providers. While ensuring personalized care of a patient, the healthcare system as a whole benefits from the practice of case management. The case manager assists in finding appropriate providers and facilities all through the continuum of services in a way that provides the best value for patient and healthcare provider.
Other functions include
- Be a part of the interdisciplinary rounds to improve case management outcomes
- Ensuring that the health insurance company understands what's happening during the patient's hospitalization.
- Provides all information the insurance company needs to approve payment for the hospitalization and works to prevent insurance claim denials
- Arranging home visits from a visiting nurse after being discharged from the hospital
- Arranging to get rehabilitation care from an inpatient rehabilitation facility
- Assisting the patient in choosing a home health company or inpatient rehab facility that's in-network with his insurer and will accept him as a patient.
- Negotiating coverage benefits between a health insurer, provider, and the patient
Case manager at a rehabilitation center
- Ensures that the patient receives necessary care at the rehabilitation center
- Helps facilitate communication between clinical staff, loved ones and community agencies to ensure continuity of care and address any questions or concerns.
- Works closely with the doctors, therapists and nurses to make sure the follow-up services will be appropriate.
- Holds Interdisciplinary meetings with patients and families to discuss their rehab goals
- Sends outcomes to the third party payers to make determinations that patients are at the appropriate level of care
- Educates staff, patients and families about options specific to care.
Case manager in a Payer-based setting (Insurance Company)
- Receives information from hospital case managers, home health care companies, physician's offices, social workers and other health care providers.
- Liaises between the provider and the insurance company
- May visit the patient at the hospital
- Provides patient and family education
- Works to meet the patient's needs while keeping an eye on the bottom line and long-term goals.
Case manager at Palliative care, home care and hospice
- Ensures that patients and those close to them experience palliative care as personalized, coherent and consistent
- Liaises with providers
- Communicates with treating physicians
- Provide patient and family education
- Assess for and organize additional services and durable medical equipment (DME)
Case manager at Workplace
A Professional case manager in a care coordination role at a workplace, delivers services to an employee who is injured on the job or who has an occupation-related illness or disability.
- Plays the care coordination role to ensure access to the right care and treatment at the optimal time.
- Identifies the most appropriate and timely resources at every phase, from diagnosis and treatment, to rehabilitation and eventual return to work and beyond.
Acquire knowledge in case management concepts, practice principles, healthcare management and delivery, healthcare reimbursement, psychosocial aspects of care, and rehabilitation
Some links to useful webinars to acquire knowledge
- Case Management Boot Camp: Strategies for Success in the Acute Care Setting and Beyond!
- Bundled Payment Review: How Case Management Can Play a Strategic Role
- Interdisciplinary Care Rounds: A Key Strategy for Improving Case Management Outcomes
- How to Think Like an Accountable Care Organization - Integrating Case Management Across the Continuum
Keep upgrading skills and make advancement
Skills believed to be critical to the success of the case manager.
- Clinical
- Communication
- Time management
- Decision-making and problem-solving
- Organizational
- Autonomy
- Conflict resolution
- Teamwork
- Delegation
- Political savvy
- Tolerance
- Commitment
- Role modeling
- Teaching
- Cultural sensitivity
Attend the 'Case Management Boot Camp: Strategies for Success in the Acute Care Setting and Beyond!' to the skills to succeed as a case manager or social worker in the new era of value-based reimbursement and accountable care. Because things are changing so rapidly, it can be a challenge to stay current and knowledgeable in the issues that most greatly impact your role as an acute care case manager or social worker. Reimbursement has changed dramatically as has utilization management, transitional planning and compliance. The Centers for Medicare and Medicaid Services (CMS) has incorporated changes that impact on payments related to readmissions, length of stay and cost of care. Who is in a better place to address these issues than case managers and social workers! Finally, how do you measure your impact on the cost and quality of care and the reimbursement your organization receives for that care? All these topics and more will be covered in this jam-packed one-day program.
The speaker Toni G. Cesta, Ph.D., RN, FAAN is Partner and Health Care Consultant in Case Management Concepts, LLC, a consulting company which assists institutions in designing, implementing and evaluating acute care and community case management models, new documentation systems, and other strategies for improving care and reducing cost. The author of nine books, and a frequently sought after speaker, lecturer and consultant, Dr. Cesta is considered one of the primary thought leaders in the field of case management. Dr. Cesta writes a monthly column called "Case Management Insider" in the Hospital Case Management journal in which she shares insights and information on current issues and trends in case management.






